Translate this page into:
Adaptive health technology assessment informing guidelines

*Corresponding author: Kriti Shukla, Center for Health Outcomes Research and Economics and South Asia Centre for Disability Inclusive Development and Research (SACDIR), Indian Institute of Public Health, Hyderabad, Telangana, India. kriti.shukla@iiphh.org
-
Received: ,
Accepted: ,
How to cite this article: Shukla K, Ghosh S. Adaptive health technology assessment informing guidelines. IHOPE J Ophthalmol. 2024;3:55-8. doi: 10.25259/IHOPEJO_4_2024
Abstract
In the present era, global decision-makers encounter numerous challenges when it comes to allocating optimal health care to their populations, primarily due to limited resources. While technology has seen remarkable advancements, determining which technologies are useful and possess robust clinical and economic evidence is paramount for informed decision-making. Health Technology Assessment (HTA) and clinical guidelines employ health economic models to aid in this process. However, these models demand significant resources and collaborations from diverse groups of experts, bodies, and organizations. Consequently, decision-making bodies are actively exploring the adoption of adaptive HTA (AHTA) as an alternative approach. AHTA involves leveraging published decisions based on health economic modeling from other countries, allowing for more efficient utilization of available data. This article delves into the essential steps and processes employed in conducting AHTA and exemplifies its application in the oncology guidelines of the National Cancer Grid in India.
Keywords
Health technology assessment
Adaptive health technology assessment
Economic analysis
Economic evidence
Guidelines
Guideline development
INTRODUCTION
In recent times, new health care technological innovations have increased to unprecedented levels. However, their impact on health and the wider implications for national health systems are not always clear. Health systems globally are challenged to identify the best health care given the finite resources at their disposal. This is where clinical and economic evidence has become crucial in making informed choices regarding new and existing technologies.
In the 1970s, computer-assisted tomography scans were introduced, which revolutionized diagnostic decision-making, and also raised major policy implications associated with its massive cost/unit (more than 300,000 USD).[1] Concerns were also raised about its widespread use and increased radiation exposure incurred by patients.[2] Therefore, in response to decision-maker’s concerns regarding the uncontrolled diffusion of costly medical equipment, the paradigm of Health Technology Assessment (HTA) emerged.[3] Recognizing the importance of health technologies and the need to establish priorities in selecting and managing these technologies, the World Health Assembly adopted resolution 60.29 in May 2007.
HTA is a multidisciplinary process that systematically reviews the evidence and evaluates the effects and impacts of health technologies. This evaluation informs a policy decision on how these technologies can be utilized in a healthcare system.[4] The assessment process goes through a process involving analysis, appraisal, and implementation. This process includes an analysis of clinical benefit and cost-effectiveness as well as consideration of the impact on budgets, equity, and health system goals. However, conducting HTA is challenging, resource-intensive, and time-consuming for all involved. In addition, conducting HTA in the Indian context is even more difficult due to the lack of local data and limited resources in terms of time, capacity and capability.
In such a scenario, adaptive HTA (AHTA) can potentially offer a viable alternative to full HTA.[5] AHTA is a pragmatic method aimed at contextualizing or adapting available evidence on a technology’s potential safety, effectiveness, and cost-effectiveness. It uses data and evidence from HTA reports produced in other countries or contexts. This reduces the opportunity cost of the time spent on analysis and brings the evidence to decision-makers quicker, therefore freeing up time and resources to answer other questions of interest. Although the adaptation process can increase uncertainty and bias, it also increases the amount of evidence feeding into decision-making.
AHTA is suitable when there is simplicity (a clear question with straightforward comparators and elements), certainty (sufficient international evidence available that can be used to make a decision), and urgency (introduction of technology will have a high impact).
When adapting evidence, it is important to consider the transferability, adaptability, and generalizability of the results in the local context. When considering the evidence, local contextual differences such as population profile, clinical benefits, treatment costs, resource use, as well as changes in adverse events and safety profile, may lead to a change in the original recommendation.
Further paragraphs explain the AHTA methodology adopted by the National Cancer Grid (NCG), India, and their experience of using it.
THE NCG’S EXPERIENCE OF USING AHTA
The NCG was established by the Department of Atomic Energy, making the Tata Memorial Center, the coordinating center in 2013, with a mandate to provide uniform and high standards of cancer care in India. It seeks to do this by following evidence-based guidelines for the management of cancer, by increasing capacity to deliver cancer services, and by conducting multi-centric collaborative clinical research.[6] The NCG includes over 300 cancer centers across India with a strong network of research organizations, patient organizations, and advocacy groups. The need to develop clinical guidelines arose from the objective of enhancing the quality of cancer care and establishing precise quality standards for evaluating and assessing the clinical practices in cancer care. In addition, these guidelines aim to facilitate improved decision-making during disease management and reimbursement claims for improved patient outcomes.
Figure 1 illustrates the initial approach to reduce variation in cancer care across the NCG, which involved the implementation of resource-stratified guidelines. These guidelines were categorized into essential care, optimal care, and optional care based on factors such as available resources, cost-effectiveness analyses, and the best available evidence, signifying their importance.
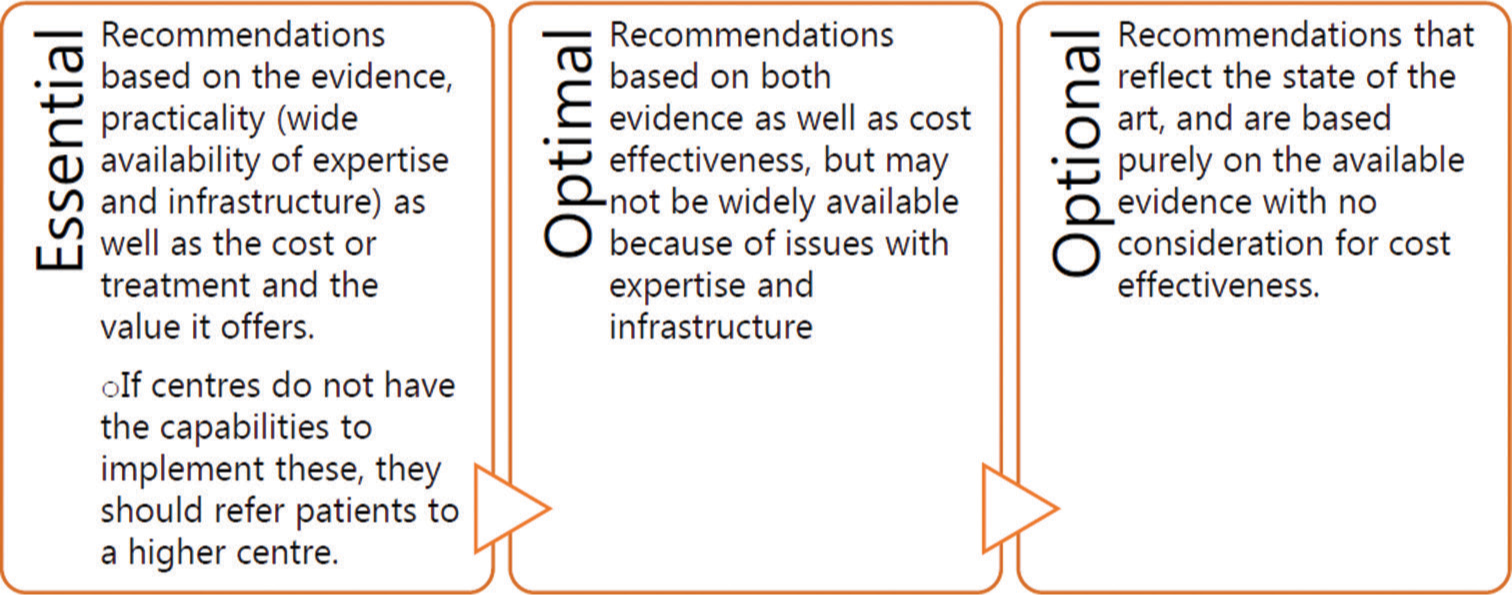
- Resource stratified guidelines. Source National Cancer Grid (NCG) guidelines, 2021.
Initially, when NCG developed the stratified guidelines, cost-effectiveness was assessed based on expert opinion rather than formal evidence. Eventually, it was agreed that formal HTA should be employed to ensure that recommendations concerning cost-effectiveness are well-informed by the evidence. However, due to the high number of interventions recommended in NCG guidelines and the difficulty in conducting HTA in the time and capacity available, it was decided to follow the AHTA approach. For AHTA, the parameters used to select the initial interventions were as follows: Common cancers and high-value interventions that are used frequently with proven efficacy.
THE NCG’S AHTA PROCESS AND METHODOLOGY
To formulate the AHTA process, a working group is convened, comprising health economists and oncologists from NCG who are familiar with the HTA processes and methods. Their role is to scope, review, and analyze the existing evidence using a stepwise approach outlined in Figure 2. Once the subject of the analysis is agreed upon, a scope document is created defining the population of interest, intervention, comparators, and relevant clinical outcomes. The scope document informed the search for evidence, and then a rapid data extraction is conducted, looking at clinical trials as well as reports on clinical benefits, toxicity and safety assessment, and cost-effectiveness studies.
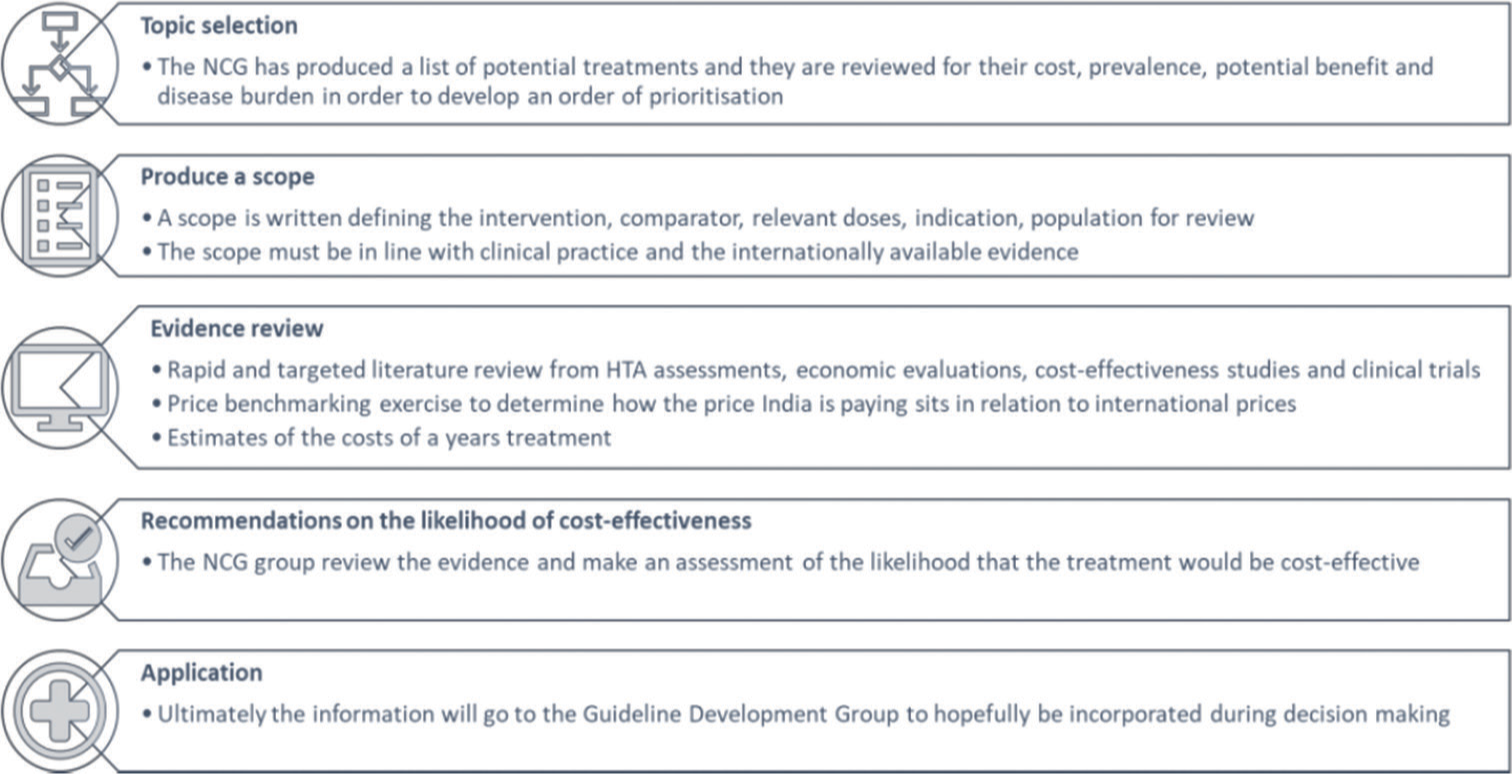
- Adaptive health technology assessment process followed at National Cancer Grid. Source NCG guidelines manual 2021.
Another step in the process is the price benchmark analysis, which provides insight into how much India is paying for interventions in comparison to the international market for the same drug and dosage. The intervention price in India is benchmarked against the international market and converted to create a ratio. Furthermore, prices are adjusted as per purchasing power parity per capita to capture the difference in income between India and other countries. This analysis is helpful in negotiating prices with manufacturers. This negotiation is possible because NCG partnered with the National Health Authority under the Ayushman BharatPradhan Mantri Jan Arogya Yojana (PMJAY) to link the optimal category of NCG guidelines with the reimbursement claim of oncology health benefits packages.
Budget analysis
The next step is to conduct a budget analysis to determine how much the intervention is expected to cost in India and what is the difference in cost when compared to the comparator on both the individual patient level and for all patients. This helps to determine the annual cost to patients and also to the PMJAY scheme, i.e., whether the yearly cost of the drug exceeds or is within the PMJAY threshold (5 lakhs/year/family).
Finally, all of the evidence aggregated is then reviewed with the Indian context in mind, and a decision is made as to whether the intervention is likely to be considered cost-effective based on feedback from the committee. To aid in transparency, a poll is conducted to capture responses to the evidence presented.
This step-wise AHTA process used by the NCG has created a systematic way to generate and assess economic evidence for an intervention which ultimately helps in drafting firm evidence-based recommendations.
DISCUSSION
AHTA is designed to save resources using existing international data and contextualizing it to local settings. While this approach can be beneficial in certain situations, it does have some limitations. The international data, while valuable, may not always accurately reflect the unique characteristics and health issues present in India. The country’s diverse population, social determinants, and healthcare infrastructure can significantly impact the effectiveness and feasibility of certain interventions.
Furthermore, AHTA relies on existing international data; it cannot assess new or unreviewed technologies that lack prior HTA evaluations.[6] This limitation is particularly relevant when considering non-pharmaceutical interventions. Nonpharmaceutical interventions include a wide range of health technologies, such as medical devices, digital health solutions, or health promotion strategies. These interventions may have unique characteristics that require thorough evaluation before implementation. Without a proper HTA process, it is challenging to ascertain their suitability, safety, and potential impact on the Indian population accurately. To address these limitations and gain a comprehensive understanding of the impact of health technologies in India, it may be a good idea to supplement international data with region-specific research and data collection.
CONCLUSION
In summation, AHTA has immense potential for augmenting and streamlining healthcare decision-making, enhancing resource allocation, and ensuring economic viability. These attributes collectively render it a valuable tool for healthcare policymakers.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Management of health technologies: An international view. BMJ. 1999;319:1293.
- [CrossRef] [PubMed] [Google Scholar]
- Computed tomography and patient risk: Facts, perceptions and uncertainties. World J Radiol. 2016;8:902-15.
- [CrossRef] [PubMed] [Google Scholar]
- Health technology assessment of medical devices Geneva: World Health Organization; 2011.
- [Google Scholar]
- Adaptive health technology assessment to facilitate priority setting in low-and middle-income countries. BMJ Global Health. 2021;6:e004549.
- [CrossRef] [PubMed] [Google Scholar]
- 2016. Available from: https://tmc.gov.in/ncg/index.php/overview/about-us [Last accessed 2022 May 02]







