Translate this page into:
Ultrasound B-scan in pediatric glaucoma

*Corresponding author: Sirisha Senthil, VST Center for Glaucoma Care, LV Prasad Eye Institute, Hyderabad, Telangana, India. sirishasenthil@lvpei.org
-
Received: ,
Accepted: ,
How to cite this article: Kolipaka GP, Senthil S. Ultrasound B-scan in pediatric glaucoma. IHOPE J Ophthalmol 2023;2:9-13.
Ever since ultrasonics have been introduced in the diagnosis of ophthalmic pathology by Mundt and Hughes,[1] various modifications and developments have taken place and with the advantage of ultrasound machines being portable, it has made its place in everyday use of ophthalmic clinical practice. Standardization of the A-scan and combining the standardized A-scan with contact B-scan probe by Ossoinig[2] led to more reliable detection and differentiation of many orbital, periorbital, and intraocular conditions both in opaque media where fundus view is obscured and in clear media as a supplement to the clinical examination. While the use of ophthalmic ultrasound in various adult ophthalmic pathologies has been widely studied and published,[3-5] there is very sparse literature about its role in pediatric cases especially in pediatric glaucomas. Children and developmentally impaired individuals may not cooperate well with other investigative modalities such as ultrasound biomicroscopy (UBM), anterior segment optical coherence tomography, computed tomography, or a magnetic resonance imaging. Ultrasound examination, on the other hand, is a simple, quick, well tolerated, and relatively inexpensive diagnostic modality that has a great potential to aid in pediatric ophthalmological practice. In this article, we would like to highlight various ways the ultrasound B-scan can be used in the diagnosis and management of pediatric glaucoma with case examples.
PRINCIPLES OF OPHTHALMIC ULTRASOUND
Ultrasound probe contains a piezoelectric ceramic crystal which when subjected to the electric pulse vibrates and produces ultrasound. Ultrasound uses acoustic waves of more than 20,000 oscillations per second and is inaudible to human ear. While abdominal ultrasound uses frequency of 5 MHz with longer wavelength, deeper penetration and lesser resolution, UBM uses a frequency of 50 MHz with shorter wavelength, and shallow penetration causing maximum resolution. Ultrasound B-scan uses 8–10 MHz of frequency with shorter wavelengths causing intermediate penetration and intermediate resolution. When the ultrasound pulse enters the eye, it is reflected by various normal and abnormal interfaces. Reflected pulse is received by the receiver. Echo is a property of the sound wave. When sound wave strikes a surface, part of it is reflected and heard as echo. After processing and amplification of the returning waves, these pulses are displayed on the display screen as echograms. Ultrasound B-scan uses two-dimensional display where the returning echo is represented as a dot and strength of the echo is represented by its brightness with the brightness being directly proportional to the strength. Gain is the procedure of increasing or decreasing the amplitude of returning echoes that are displayed on the screen. Ultrasound machine in the present day combines B-scan probe with a cross vector facility where the A-scan spikes are also generated in the area at which the cross vector is applied.
ULTRASONOGRAPHIC APPEARANCES OF NORMAL OCULAR STRUCTURES IN CHILDREN
The average axial length of a full term newborn is usually around 15–18 mm with an anterior chamber depth of 2.4–2.9 mm.[6] The eyeball continues to grow gradually until it reaches the adult axial length of 22–24 mm which is usually attained by around 4 years of age.[7]
Cornea and the anterior chamber are usually not visualized easily without adequate standoff or immersion technique. Lens in children is usually anechoic and is represented by the anterior and posterior echoes which represent the margins of the lens perpendicular to the sound beam. Posterior to the lens lies the vitreous which is usually anechoic in children [Figure 1]. The Posterior wall of the eyeball which constitutes the retina, choroid, and sclera from anterior to posterior are equally echogenic structures and are sonographically indistinguishable from each other. The posterior wall usually measures between 1 and 2 mm in thickness.[8] Beyond the sclera lies the echogenic orbital fat with a hypoechoic band extending posteriorly through the fat representing the optic nerve.
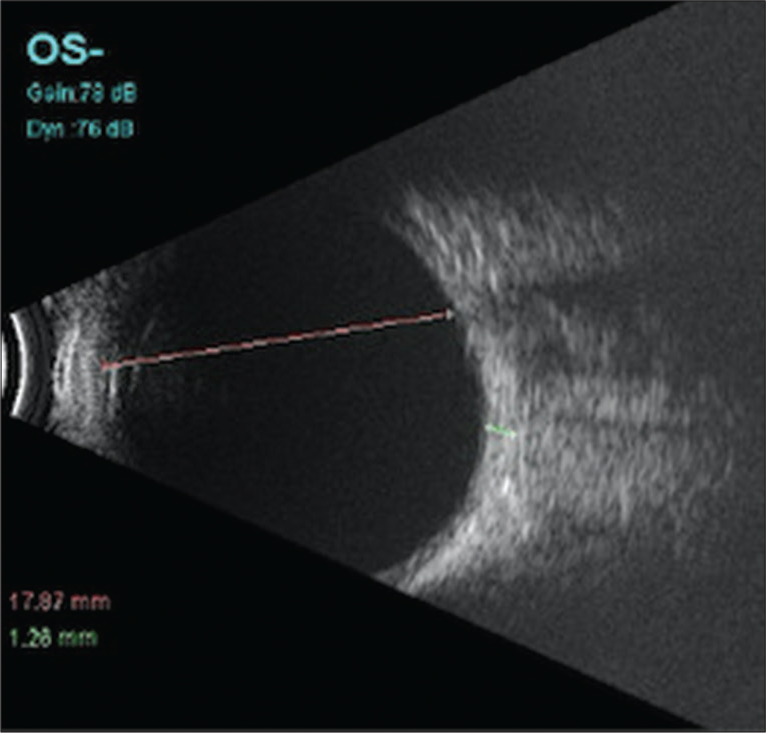
- Ultrasound B-scan of a 6-month-old child showing anechoic vitreous cavity and axial length measurement (Pink line).
APPLICATIONS OF ULTRASOUND B-SCAN IN PEDIATRIC GLAUCOMAS
Ruling out secondary causes of glaucoma preoperatively
Pediatric glaucomas can present with various signs most common of which are enlarged eyeballs or buphthalmos and corneal haziness due to epithelial corneal edema. However, a varied number of clinical conditions such as congenital hereditary endothelial dystrophy, mucopolysaccharidosis, and obstetric birth trauma can mimic these features and mislead us to the diagnosis of buphthalmos.[9-11] Furthermore, there could be associated secondary cause of the increase in intraocular pressure (IOP) causing enlargement of globes which the clinicians need to be aware of and attempt to diagnose before subjecting the child to examination under anesthesia. In one such clinical scenario, a 1-year-old boy was referred to glaucoma services of our tertiary care center, being diagnosed as right eye primary congenital glaucoma based on large eye with high IOP. On performing an ultrasound B-scan, which we routinely perform in all congenital and infantile glaucoma at first presentation, a heterogeneous retinal lesion with calcifications and high reflective echoes in the vitreous was noted which was suggestive of retinoblastoma [Figure 2]. Retinoblastoma, being the most common intraocular malignancy in childhood, can have different types of clinical presentations including leukocoria, strabismus, proptosis, anterior chamber inflammatory signs, and secondary glaucoma.[10] Although leukocoria and strabismus are usually the most common clinical presentation,[11] retinoblastoma can also present as buphthalmos with increased corneal diameter and high IOP.[12,13] Tumor on B-scan presents as a heterogeneous mass arising from the retina, obliterating the vitreous cavity with attachment of the mass to the posterior wall of the globe. These tumors usually demonstrate high internal reflectivity although the amount of reflectivity depends on the amount of calcification. Calcification can be seen in about 50–80% of cases of retinoblastoma[14,15] but if present confirms the diagnosis. Ultrasound in this case helped in the diagnosis of the condition of the child even before subjecting them to examination under anesthesia. The child was then referred to oculoplastic services and treated appropriately.
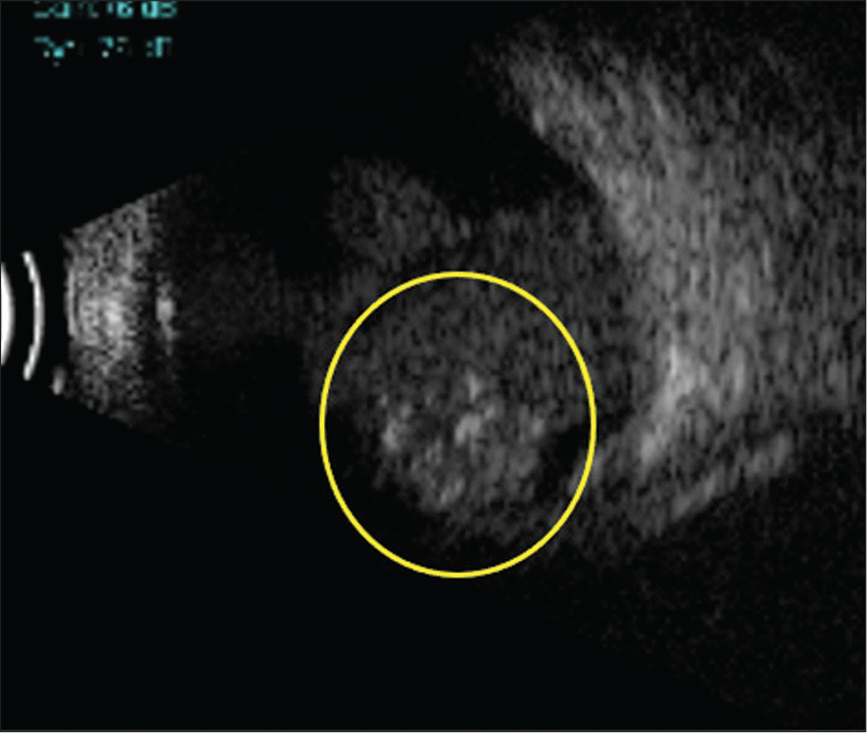
- Ultrasound B-scan showing a heterogeneous retinal lesion with calcifications and high reflective echoes in the vitreous suggestive of retinoblastoma (yellow circle).
Diagnosing associated posterior segment pathologies
Surgical interventions in patients with Sturge-Weber syndrome (SWS) can be associated with increased risks of serious intra and post-operative complications such as choroidal effusions and suprachoroidal hemorrhages. The possibility of these complications increases when SWS is also associated with choroidal hemangioma which is present in around 20–70% of the cases.[16] Pre-operative ultrasound B-scan in patients with SWS can reveal an underlying choroidal hemangioma in the form of increased choroidal thickness [Figure 3] before taking up any surgical intervention, to alert the surgeon about the possibility of serious and sight-threatening complications during and after surgery, and helps to plan and take appropriate measures to prevent them. Kaushik et al.[17] reported perioperative use of oral propranolol in a dosage of 2 mg/kg body weight in patients with choroidal hemangiomas to minimize the complications.
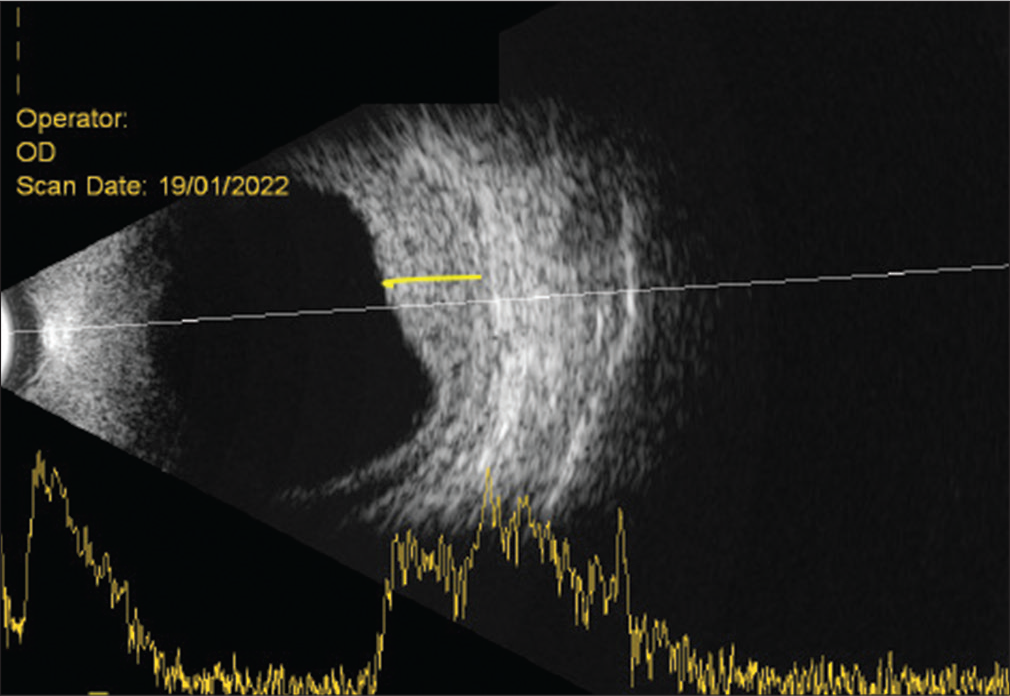
- Ultrasound B-scan in a patient with Sturge-Weber syndrome with an underlying choroidal hemangioma in the form of increased choroidal thickness (yellow line).
Diagnosing and following up on post-operative complications
Choroidal detachments can occur as a sequel to any intraocular surgery more commonly with glaucoma surgeries. They can be serous or hemorrhagic. Clinically, choroidal detachments appear as smooth and dome shaped elevations and can be single or multiple. In children where clinical examination cannot be adequate due to poor cooperation, ultrasound B-scan plays a very important role in not only diagnosing but also helping in differentiating the type of choroidal detachment, and monitoring the response to treatment. Ultrasonographically, choroidal detachments appear as smooth and dome like elevations that usually do not extend beyond the equator. The space behind the membrane is echoluscent in serous choroidal detachments [Figure 4a] or can have multiple moderate to high reflective dot like echoes in case of hemorrhagic choroidal detachments [Figure 4b]. Serial ultrasound examinations can help in detecting the resolution of choroidal detachment and clot lysis in hemorrhagic choroidal detachments which helps in planning the timing for drainage. Change in the contour of the choroidal detachment from convex to concave indicates that the hemorrhage or the detachment is resolving [Figures 5a-d]. It also helps to evaluate associated retinal complications if any.
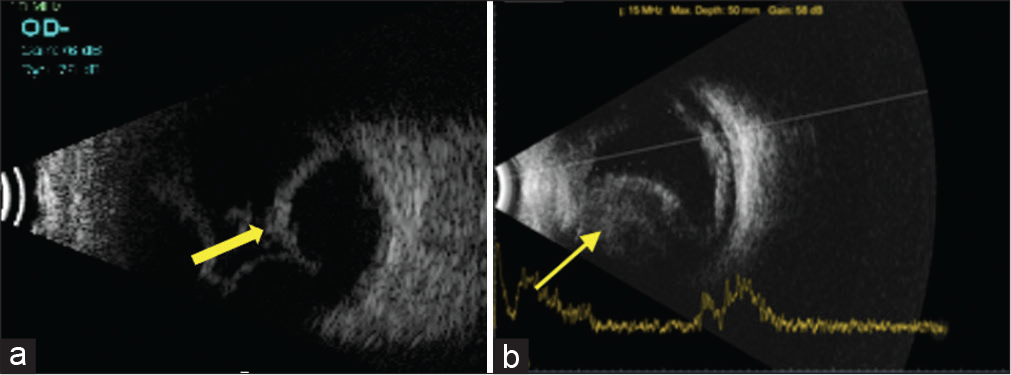
- (a) Ultrasound B-scan showing smooth and dome like elevations not extending beyond the equator with echoluscent space behind the membrane in serous choroidal detachment (yellow arrow). (b) Multiple moderate-to-high reflective dot like echoes are seen in hemorrhagic choroidal detachment (yellow arrow).
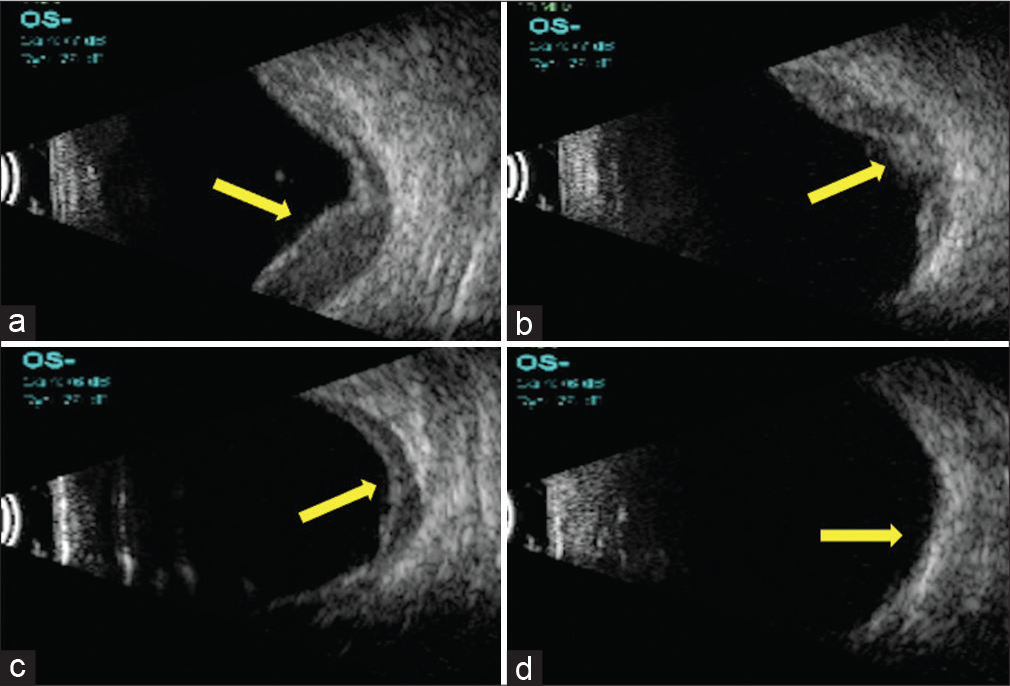
- (a-d) Series of ultrasound B-scan pictures showing change in the contour of the choroidal detachment from convex to concave indicating that the hemorrhage or the detachment is resolving (yellow arrows).
Measurement of axial length to monitor progression in eyes with congenital glaucoma
Careful follow-up is very essential for pediatric glaucoma especially post-surgery. As children may not cooperate for IOP measurement at every visit and frequent anesthesia is not possible, detection of progression of glaucoma by means of other cues plays a very important role. Serial axial length measurement by ultrasonography as a means of glaucoma progression detection has been advocated by many authors.[18-20] The difficulty in monitoring only with IOP is not appropriate as the eyeball can enlarge in size as a response to elevated IOP, which may intern result in normal IOP and miss progression. Any abnormal or abrupt change in the axial length beyond that expected for age should raise the suspicion of elevated IOP.
Post-glaucoma drainage implant surgery follow-up
Lloyd et al.[21] initially described the echographic evaluation of the filtering blebs post-glaucoma drainage device. As evaluating the filtering blebs postoperatively may not be feasible in every case especially in pediatric glaucoma, ultrasound can aid as a useful adjunct. Fluid around the implant within the bleb is seen on B-scan ultrasound as echoluscent area surrounding the plate which is an echogenic structure [Figure 6]. Although the amount of IOP may not be determined by bleb morphology, the presence of fluid around the implant indicates a functioning tube without any blockage. Serial ultrasonography can help in follow-up of the patient’s post-drainage device implantation. For example, in a 6-year-old kid, who is a case of medically uncontrolled glaucoma in pseudophakia, a non-valved Aurolab Aqueous Drainage device was implanted. At 1-week post-operative visit, ultrasound B-scan detected a hypoechoic bleb devoid of any fluid [Figure 7a]. At week 6 post-operative visit, a large echoluscent fluid filled reservoir with central hyperechogenicity indicating implant surrounded by fluid reservoir was noted confirming that the ligature has opened up [Figure 7b]. At 2-month post-operative visit, the IOP was low at 2 mm Hg and B-scan ultrasonography revealed kissing choroidal detachment [Figure 7c] Due to non-resolving choroidal detachment on serial ultrasonography, the child was taken up for tube ligature. Post-tube ligature B-scan revealed that choroidal detachment was resolved and fluid around the implant was noted [Figure 7d]. Ultrasound B-scan played a very important role at every stage in the diagnosis and follow-up of this complication in this patient.
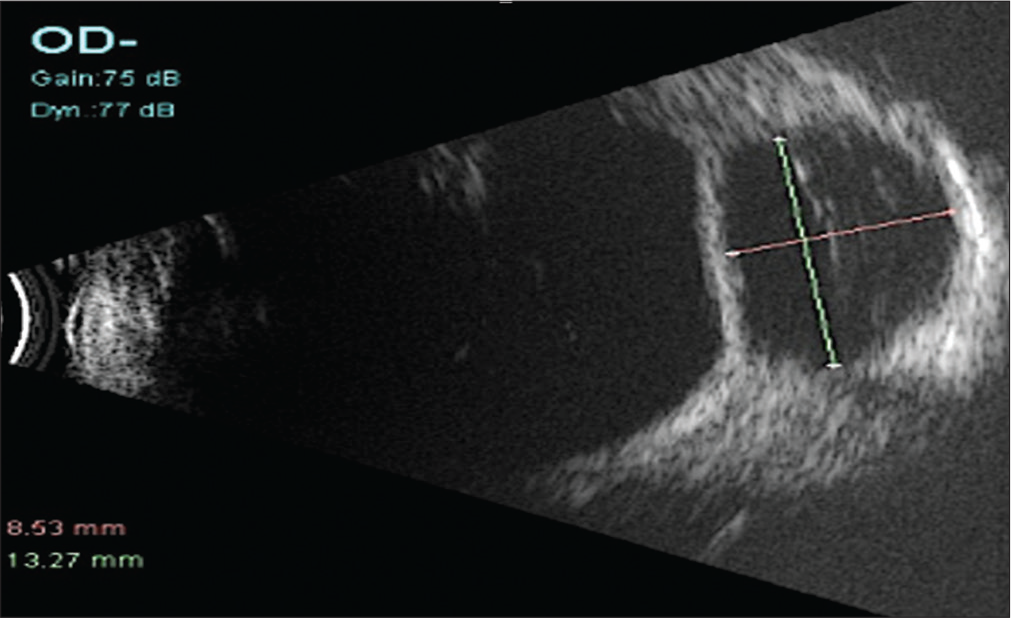
- Echoluscent area surrounding the plate which is an echogenic structure indicating the fluid around the implant within the bleb along with the horizontal and vertical measurements (green and pink lines) of the bleb on B-scan ultrasound.
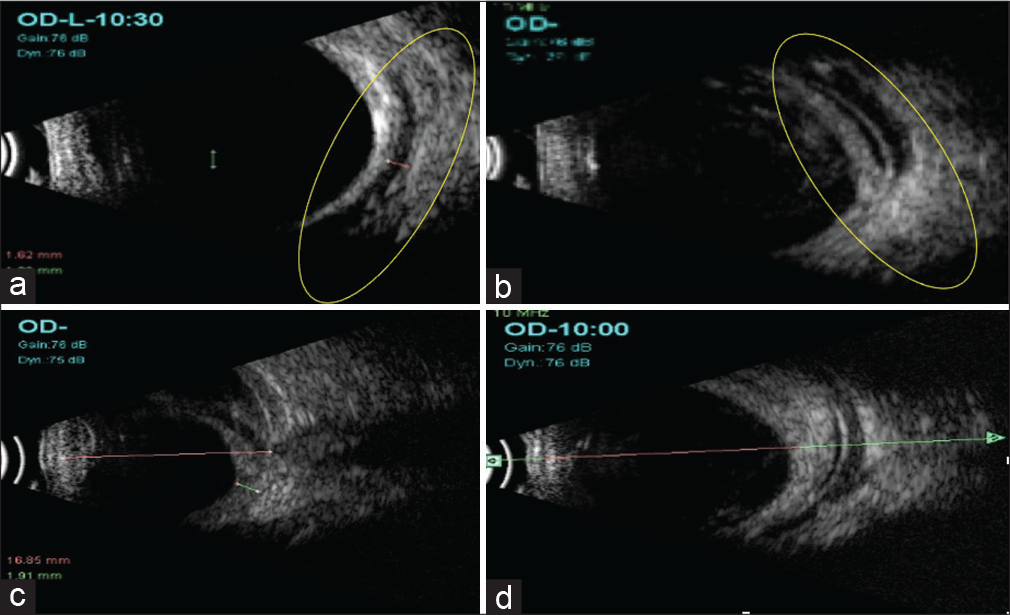
- (a) Ultrasound B-scan showing a hypoechoic bleb devoid of any fluid (yellow circle) seen at 1-week post-operative visit off AADI implantation. (b) Ultrasound B-scan showing a large echoluscent fluid filled reservoir with the central hyperechogenicity (yellow circle) \indicating implant surrounded by fluid reservoir was noted confirming that the ligature has opened up at week 6 post-operative visit. (c) At 2-month post-operative visit, B-scan ultrasonography revealed kissing choroidal detachment. (d) Post-tube ligature B-scan revealed that choroidal detachment was resolved and fluid around the implant was noted.
Baig et al.[22] in their retrospective case series evaluated the cases in which B-scan ultrasonography was performed in assessing the glaucoma drainage device patency and function placed in refractory pediatric glaucomas. They found it to be very useful especially in cases where the tube tip was not visualized due to opaque corneas, when IOP was elevated and when the bleb was not visualized. Alonzo et al.[23] reported a case of 18-month-old girl with primary congenital glaucoma with multiple previous surgeries including Ahmed glaucoma valve implantation who presented with sudden increase in the size of the eye. She was diagnosed with increasing buphthalmos and was started on AGM until B-scan ultrasonography revealed a fluid filled reservoir pushing the globe forward. She subsequently underwent cyst removal with AGV replacement.
To conclude, Ultrasound B-scan is a simple, easily available, and cost-effective modality that has the potential to greatly reduce the number of examinations under anesthesia in children and serve as a useful adjunct to clinical examination.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Ultrasonics in ocular diagnosis. Am J Ophthalmol. 1956;41:488-98.
- [CrossRef] [PubMed] [Google Scholar]
- Standardized echography: Basic principles, clinical applications, and results. Int Ophthalmol Clin. 1979;19:127-210.
- [CrossRef] [PubMed] [Google Scholar]
- Pictorial essay: B-scan ultrasonography in ocular abnormalities. Indian J Radiol Imaging. 2009;19:109-15.
- [CrossRef] [PubMed] [Google Scholar]
- New applications in ultrasound technology. Br J Ophthalmol. 1999;83:1246-9.
- [CrossRef] [PubMed] [Google Scholar]
- The use of dynamic ultrasound B-scan to detect retinal tears in spontaneous vitreous haemorrhage. Eye. 1995;9:502-6.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasonic measurements of the eye in the newborn infant. Acta Ophthalmol (Copenh). 1979;57:1048-56.
- [CrossRef] [PubMed] [Google Scholar]
- Axial length in apparently normal pediatric eyes. Eur J Ophthalmol. 2014;24:120-3.
- [CrossRef] [PubMed] [Google Scholar]
- B mode ultrasonography-spectrum of paediatric ocular disease. Eur J Radiol. 1998;26:132-47.
- [CrossRef] [PubMed] [Google Scholar]
- Conditions that can be mistaken as early childhood glaucoma. Ophthalmic Genet. 2011;32:129-37.
- [CrossRef] [PubMed] [Google Scholar]
- Different Types of clinical presentations and stages of retinoblastoma among children. Cureus. 2020;12:e10672.
- [Google Scholar]
- Clinical presentation of intraocular retinoblastoma; 5-year hospital-based registry in Egypt. J Egypt Natl Cancer Inst. 2015;27:195-203.
- [CrossRef] [PubMed] [Google Scholar]
- Phthisis bulbi and buphthalmos as presenting signs of retinoblastoma: A report of two cases and literature review. Eur J Ophthalmol. 2006;16:465-9.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral retinoblastoma presenting with simultaneous phthisis bulbi and buphthalmos. J Pediatr Ophthalmol Strabismus. 2003;40:161-3.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasonography of ocular tumours. Indian J Radiol Imaging. 2007;17:8-10.
- [CrossRef] [Google Scholar]
- Ultrasonic findings in intraocular retinoblastoma and correlation with histopathologic diagnosis. Int Ophthalmol. 1995;19:71-5.
- [CrossRef] [PubMed] [Google Scholar]
- Hemangioma of the choroid. A clinicopathologic study of 71 cases and a review of the literature. Surv Ophthalmol. 1976;20:415-31.
- [CrossRef] [PubMed] [Google Scholar]
- Perioperative propranolol: A useful adjunct for glaucoma surgery in sturge-weber syndrome. Ophthalmol Glaucoma. 2019;2:267-74.
- [CrossRef] [PubMed] [Google Scholar]
- Correlation of postoperative axial length growth and intraocular pressure in congenital glaucoma--a retrospective study in trabeculotomy and goniotomy. Graefes Arch Clin Exp Ophthalmol Albrecht Von Graefes Arch Klin Exp Ophthalmol. 2001;239:893-9.
- [CrossRef] [PubMed] [Google Scholar]
- Evolution of axial length in congenital glaucoma. Invest Ophthalmol Vis Sci. 2012;53:6766.
- [Google Scholar]
- Axial length changes following surgical intervention in children with primary congenital glaucoma. Front Ophthalmol. 2021;1:747801.
- [CrossRef] [Google Scholar]
- Echographic evaluation of glaucoma shunts. Ophthalmology. 1993;100:919-27.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound evaluation of glaucoma drainage devices in children. J AAPOS. 2015;19:281-4.
- [CrossRef] [PubMed] [Google Scholar]
- Proptosis masquerading as buphthalmos following glaucoma drainage device surgery in a child with congenital glaucoma. J AAPOS. 2018;22:475-7.e1.
- [CrossRef] [PubMed] [Google Scholar]






