Translate this page into:
The pattern of ocular disorders in eye patient attendants in tertiary eye care centers

-
Received: ,
Accepted: ,
How to cite this article: Khan A, Singh M. The pattern of ocular disorders in eye patient attendants in tertiary eye care centers. IHOPE J Ophthalmol 2023;2:73-6.
Abstract
Objectives:
This study aims to assess the pattern of ocular disorders in patient attendants at tertiary eye care centers.
Materials and Methods:
A cross-sectional study has been conducted at a tertiary eye care center in northern India. The study participants were adults aged 18 years who came along with patients. The study duration was from September 2022 to March 2022. This study was conducted to assess the ocular disorder inpatient attendant. The survey methods included the Bruckner test and torchlight examination.
Results:
A total of 202 subjects were assessed in our study. Of them, 71 (35.1%) were diagnosed with emmetropia. Refractive errors for distance were reported in 120 (59.4%) attendants. Of them, 104 (51.4%) did not have any previous eye disease, 81 (77.88%) were unaware, and 23 (22.11%) were aware of their ocular disorder.
Conclusion:
The majority of attendants who did not have any ocular symptoms and also never underwent any eye examination were suffering from eye disease. We found that there was a high significance between attendant ocular symptoms (without previous examination) and awareness (P = 0.05).
Keywords
Ocular disorder
Bruckner test
Descriptive analysis
Opportunistic screening
Patient attendant
INTRODUCTION
International surveys conducted over the last few decades have ensured that caregivers who provide care to patients experience a great deal of stress.[1,2] The majority of the literature on this topic has been done on the assessment of caregivers of patients with intractable neurological diseases (e.g., Alzheimer’s and Parkinson’s disease).[3] One of the studies found that, although uncorrected refractive errors are a major cause of visual impairment and blindness globally, the level of knowledge about this issue and its correction methods is low in the north Indian region.[4] Previous studies have been conducted to determine the psychological status of patient attendants or caregivers, but they did not examine their eye and awareness status. Most people are unaware of their eye condition, and it could be due to a variety of reasons, that is, lack of knowledge, economic concern, a negative attitude toward eye health, or minimal or fewer symptoms. The objective of this study is to assess the ocular and awareness status of the attendant.
MATERIALS AND METHODS
This study was a cross-sectional descriptive study with convenient sampling. The study was approved by the institutional ethics committee and adhered to the tenets of the Declaration of Helsinki. The study population consisted of patient attendants available in the study area. We obtained the written consent of the patient’s attendant before taking them into our study. Attendants aged more than 18 years and willing to participate were included in the study. Optometrists (B. Optom with more than 5 years experience) helped collect the data, and they were not aware of the study in OPD. The Binocular Bruckner test was performed without spectacle correction, if any. Direct ophthalmoscopes (Beta 200; Heine Optotechnik Germany) for Bruckner tests and torch light examinations were performed in all subjects, and results were recorded. Emmetropia was defined as a bright crescent <2 mm in size visible superiorly in the pupillary area. Myopia was defined as a bright crescent >1 mm in size visible inferiorly in the pupillary area. Hyperopia was defined as a bright crescent >2 mm in size visible superiorly in the pupillary area. Astigmatism was defined as a bright inferior crescent >1 clock hour in the pupillary area of an eye with myopic astigmatism.[5,6] An attendant was considered myopic if at least one eye was myopic and hyperopic if at least one eye was hyperopic, but neither was myopic. A Torchlight examination has been conducted. Both Bruckner and the torchlight exam were performed under binocular viewing conditions. D Both Bruckner and the torchlight exam were performed under binocular viewing conditions. The data were analyzed using Statistical Package for the Social Sciences (SPSS) version 20 (SPSS Inc., Chicago, IL, U.S.A.). Simple descriptive and inferential statistics were done. Descriptive statistics were done, with results presented as frequencies, proportions, mean, and standard deviations. The Chi-square test was used to test associations between patient attendant characteristics and their awareness status. A significant level was set at P = 0.05.
RESULTS
A total of 202 attendants were screened. The males were 153 (75.7%), and the females were 49 (24.3%). The caregivers were parents (7.4%), spouses (23.8%), siblings (10.4%), children (32.7%), and others (relatives and friends) (25.8%) ages between 18 and 80 [Table 1].
| n | Percentage | |
|---|---|---|
| Male | 153 | 75.7 |
| Female | 49 | 24.3 |
| Relation with patient | ||
| Parents | 15 (7.4) | |
| Siblings | 21 (10.4) | |
| Spouse | 48 (23.8) | |
| Children | 66 (32.7) | |
| Other | 52 (25.7) |
n: Number of participants
A total of 63 (31.1%) attendants were emmetropic in both eyes. Refractive errors for distance were reported in 120 (59.4%) attendants. Of them, 8 (6.6%) were diagnosed with refractive error for distance in one eye and 113 (94.13%) in both eyes. In both eyes, hyperopia was reported in 20 (16.6%) attendants, followed by myopia in 28 (23.3%) attendants, and astigmatism in 72 (60%) attendants. Eight (6.6%) attendants were identified with refractive errors in one eye. Of them, 6 (5%) were identified with hyperopia, 1 (0.83%) with myopia, and 1 (0.83%) with Astigmatism [Table 2 and Figure 1].
| Types of refractive error | Right eye (%) | Left eye (%) |
|---|---|---|
| Emmetropia | 71 (35.1) | 63 (31.2) |
| Astigmatism | 71 (35.1) | 72 (35.6) |
| Myopia | 27 (13.4) | 28 (13.9) |
| Hypermetropia | 14 (6.9) | 20 (9.9) |
| Other | 19 (10.5) | 19 (10.4) |

- Bruckner test status.
A total of 26 (12.9%) attendants were previously diagnosed with presbyopia in their last comprehensive examination. Strabismus was diagnosed in 3 (1.5%) attendants. The two attendants were diagnosed with one eye deviation (exotropia) at 19 and 61 years old, and one attendant with both eyes (esotropia) at 35 years old [Table 3]. Other 19 (10.5%) subjects include cataracts in 16 (7.9%) subjects; pterygium in 2 (1%) subjects; and watering complaints in 1 (0.5%) subject. A total of 54 (26%) attendants were taking treatments for their eye disease, and 149 (74%) were not taking any type of treatment for their eye problems [Figure 2].
| Types of deviation | Right eye (%) | Left eye (%) |
|---|---|---|
| Esotropia | 1 (0.5) | 1 (0.5) |
| Exotropia | 1 (0.5) | 1 (0.5) |
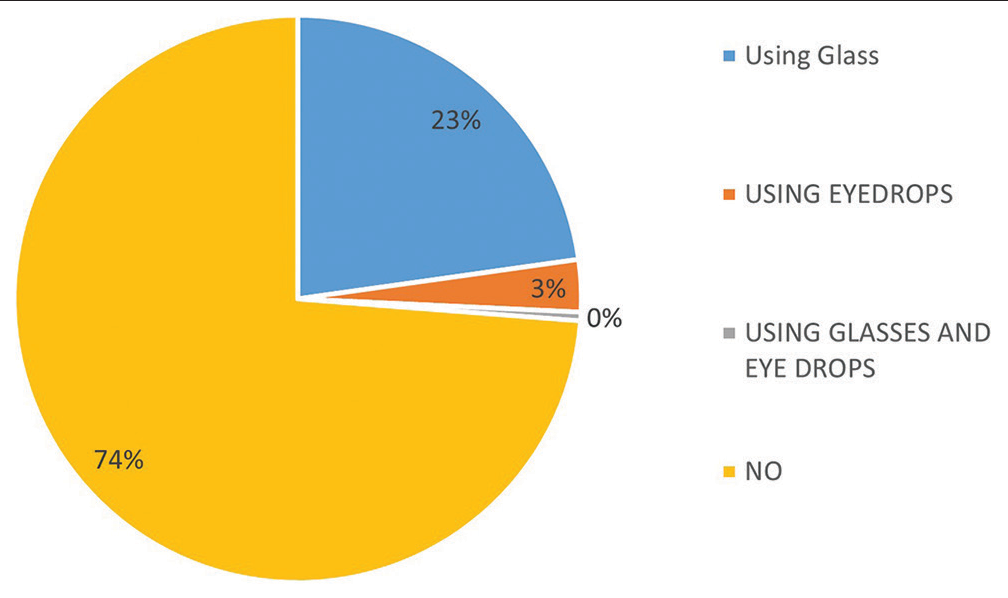
- Taking any eye treatment.
A total of 81 (40.1%) attendants were aware of their ocular condition, and 121 (59.9%) were unaware. Of the attendants with previous eye problems, 58 were aware and 40 were unaware; of the attendants without previous eye problems, 23 were aware and 81 were unaware. There was a high significance between awareness status and previous eye problems with P < 0.05 [Table 4 and Figure 3].
| Previous eye problem | Aware | Unaware | Total |
|---|---|---|---|
| Yes | 58 | 40 | 98 |
| No | 23 | 81 | 104 |
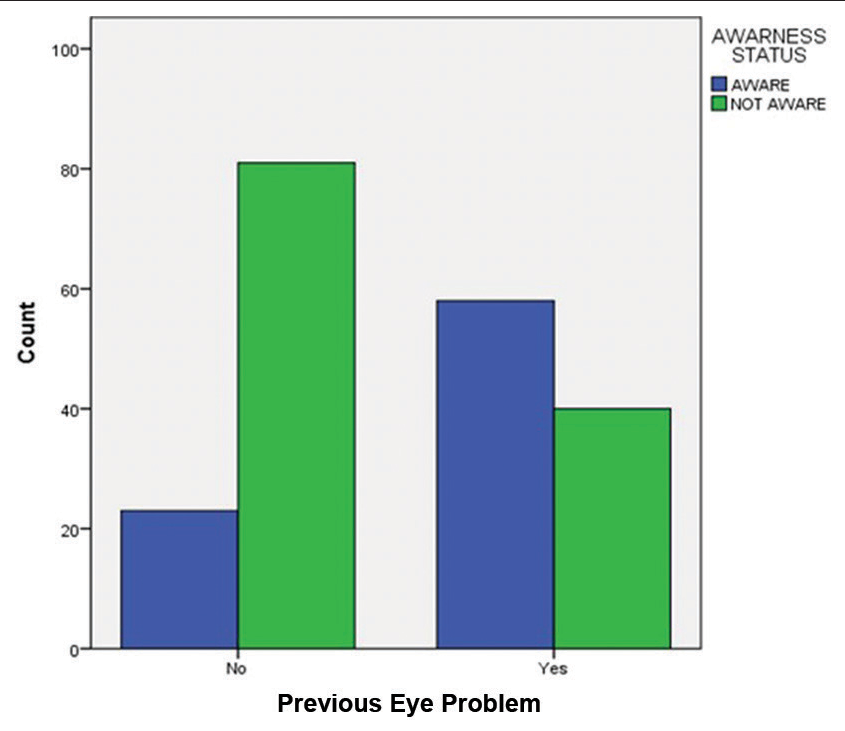
- Awareness status based on the previous eye problem.
DISCUSSION
As previously said, the Bruckner test is simple, quick, reliable, and easy to administer to all age groups, so we used this method as a tool in this study.[7] In our study, most attendants were parents, children, or spouses of these patients. This shows that close family members were unaware of their eye health. These attendants spent the most time with their sick relatives and saw them suffer from visual abnormalities. But still, most of them did not undergo any ophthalmic examination. Attendants of ophthalmic patients have suffered from a variety of refractive errors, and they are unaware of their ocular conditions, especially when they did not have any previous eye problems (P = 0.05). Our study found that attendants who are suffering from previous eye problems have ocular symptoms too, but they never did their eye examination, which may indicate that people have a financial crisis and/or negative attitudes towards eye health. This shows the need for economic empowerment, financial support, and awareness towards eye health for these attendants (as the previous study also suggests),[8] and routine screening for awareness is required to enhance the eye check-up. Between attendant socio-demographic characteristics and awareness, like the relationship between education. It could be due to the small sample size and unequal distribution of rural and urban populations, which can be limitations for our study. As per the literature, most studies have been conducted to determine the psychological status of patient attendants or caregivers, whether they are from an ophthalmic or systemic background, and in our study, we have assessed the ocular or clinical status of the attendant’s eye.[9] Furthermore, more focus should be directed toward enhancing eye screening and awareness and changing negative attitudes toward eye examination.
CONCLUSION
In this study, we found that the majority of the patient attendants also had eye disorders, but they were not symptomatic or aware of their eye health, and for this reason, they delayed the examination.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist. 1980;20:649-55.
- [CrossRef] [PubMed] [Google Scholar]
- End-of-life care and the effects of bereavement on family caregivers of persons with dementia. N Engl J Med. 2003;349:1936-42.
- [CrossRef] [PubMed] [Google Scholar]
- Care burden and depression in caregivers caring for patients with intractable neurological diseases at home in Japan. J Neurol Sci. 2009;276:14852.
- [CrossRef] [PubMed] [Google Scholar]
- Spirituality and meaning in supportive care: Spirituality and meaning-centered group psychotherapy interventions in advanced cancer. Cancer. 2002;10:272-80.
- [CrossRef] [PubMed] [Google Scholar]
- Can the Brückner test be used as a rapid screening test to detect significant refractive errors in children? Indian J Ophthalmol. 2007;55:213-5.
- [CrossRef] [PubMed] [Google Scholar]
- Patterns of presentations at a free eye clinic in an urban state hospital. Niger J Clin Pract. 2013;16:145-8.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of Brückner's test for screening of refractive errors by non-ophthalmologist versus ophthalmologist: A comparative study. Middle East Afr J Ophthalmol. 2020;26:185-8.
- [CrossRef] [PubMed] [Google Scholar]
- Burden of family caregivers of ophthalmic patients in a university teaching hospital in south-west Nigeria. Malawi Med J. 2019;31:39-44.
- [CrossRef] [PubMed] [Google Scholar]
- The psychological health of patients and their caregivers In: Marsh D, ed. Orthogeriatrics: The management of older patients with fragility fractures (2nd ed). Cham: Springer; 2021. Ch. 13
- [CrossRef] [PubMed] [Google Scholar]






