Translate this page into:
Refractive status seen amongst school pupils with vernal keratoconjunctivitis in Jos East Local Government Area of Plateau State, North - Central Nigeria

*Corresponding author: Panshak Elisha Tenmang, Department of Ophthalmology, Jos University Teaching Hospital, Jos, Nigeria. Panshak_tenmang@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Tenmang PE, Ramyil AV, Wabare SZ, Kadala N, Kopse GS, Wade PD. Refractive status seen amongst school pupils with vernal keratoconjunctivitis in Jos East Local Government Area of Plateau State, North - Central Nigeria. IHOPE J Ophthalmol 2023;2:68-72.
Abstract
Objectives:
This study aims to determine the types of refractive errors commonly seen in patients with Vernal keratoconjunctivitis (VKC) among the pupils in the Jos East Local Government area of Plateau State, Nigeria.
Materials and Methods:
A school-based descriptive study using a multistage sampling technique was carried out for 4 months. The visual acuity of the pupils was checked using a non-illuminated Snellen’s chart at 6 m, assessing one eye at a time. Individuals with visual acuity worse than 6/12 had pinhole tests and refraction done. Statistical analysis was done using Statistical Package for the Social Sciences version 20 and frequencies, simple percentages, and Chi-square were used to compare proportions.
Results:
A total of 400 participants were seen during the study, out of which 84 participants had vernal keratoconjunctivitis. Of these, 51 (60.7%) had refractive errors. Astigmatism was the most common form of refractive error seen in our study 26 (31%), myopia was seen in 15 (17.9%) whereas hypermetropia was the least seen in 10(11.9%). Simple astigmatism was seen more in individuals with acute stage of VKC 9 (75.0%) whereas compound astigmatism was commonly seen in participants with chronic stage of VKC (42.9%).
Conclusion:
Astigmatism was the commonest form of refractive error seen in these patients and simple astigmatism was the commonest variant of astigmatism seen.
Keywords
Refractive status
Vernal keratoconjunctivitis
School pupils
Astigmatism
INTRODUCTION
Vernal keratoconjunctivitis (VKC) is a chronic, bilateral, recurrent, and self-limiting allergic inflammation of the conjunctiva which has a periodic seasonal incidence.[1] It is mainly believed to be a disease of childhood; the mean age of presentation is 12 years and mostly resolves after puberty, usually around 4–10 years after onset. The disease is more prevalent among males, with the male-to-female ratio varying from 4:1 to 1.3:1.[2,3] Major characteristics of the disease include itching, redness, discomfort, stringy discharge, photophobia, burning and stinging, giant papillae on the upper tarsal conjunctiva, superficial keratopathy, corneal shield ulcers, and keratoconus leading on to permanent corneal damage.[2] A family history of atopy is seen in 49% of patients with VKC. Patients with VKC may also have a medical history of other atopic conditions including asthma (26.7%), rhinitis (20%), and eczema (9.7%), and show no evidence of infection.[4,5] Vision-threatening complications such as keratoconus, corneal scarring, refractive errors, shield ulcers, and treatment-related complications such as steroid-induced glaucoma make VKC to be of greater concern.[2] All forms of refractive errors have been reported in different studies with varying degrees of involvement. A study done by Bangal et al. and Chaudhary et al. reported astigmatism to be the most common form of refractive error in VKC, whereas Shetty et al. reported hypermetropia to be the most common form of refractive error seen among patients with VKC.[6-8] The impact of refractive on the quality of life and productivity of the child can be extensive, affecting the educational, economic, and social life of the child.[9] The academic performance as well as social interaction of the child can be affected when their vision is impaired.[10]
To the best of the author’s knowledge, there is no study on the refractive status of school children with VKC in Jos East Local Government Area of Plateau State. This study seeks to establish the types of refractive errors seen in school children with VKC in this area so that they can be easily corrected and also provides a baseline date for future interventions.
MATERIALS AND METHODS
This was a school-based cross-sectional descriptive study conducted over 4 months from October 2019 to January 2020 in Jos East LGA of Plateau State. The population for the study consisted of children enrolled in all primary schools within the LGA with a total of 113 primary schools of which 76 were public and 37 private. The total enrolment was 22,812, as of the 2019/2020 academic session, out of which 19,698 were enrolled in public primary schools while 3114 were enrolled in private primary schools. These schools are divided into five educational districts, namely, Maigemu, Fobur, Shere, Fursum, and Federe. The list of grouped schools was obtained from the Education Authority. A multistage sampling technique was used to select the schools. From each district, five schools were chosen randomly by balloting from the list of schools. In each school, a class was chosen randomly by balloting from each arm running through primary one to primary six systemic random was used to recruit 16 students from each class depending on the number of students present at school on the day of the study, those not present in school were regarded as absent. A sampling interval was then determined by dividing the number of students in class by 14 using the class register, simple random sampling by balloting was used to determine which student to recruit first on the class register where numbers were written on folded papers and the class teacher was made to pick one and open, whichever number the teacher gets to pick was the first to be recruited and subsequently the sampling interval determined was added to this to determine the next student to be recruited until a total of 14 was recruited from each class. Using Fisher’s formula for sample size determination of a cross-sectional study, a minimum sample size was calculated to 360; however, a total of 400 participants were recruited for the study.
Permission for the study was obtained from the Ethical and Research Committee of the Jos University Teaching Hospital, and Plateau State Ministry of Education through the Area Inspectorate of Education in Jos East LGA. Written and signed consent was obtained from parents/guardians of the pupils authorizing their children/wards to participate in the study. Furthermore, assent was obtained from the pupils who participated in the study after explaining to them what the study was all about and the benefits of participating.
A self-developed semi-structured, interviewer-administered questionnaire with sections on demographic data of the pupil, clinical, medical, and family history was used as the instrument for the study. Other instruments used included a non-illuminated Snellen chart, non-illuminated tumbling E-chart, pen torch, 2% fluorescein strip, direct ophthalmoscope, magnifying loupe 2X, Jackson cross cylinder, stationery, 0.5% amethocaine, cotton wool, pen torch with a blue filter, and a 6 m rope, pinhole occluder, auto-refractometer, cyclopentolate, and trial lens box with the adjustable pediatric trial frame. The pupils were examined and distant visual acuity was tested for each pupil using the non-illuminated Snellen chart at 6 m from the child by the research assistant. This procedure was explained to the pupils to understand as it is a test to help us know the function of their eyes and there is no need for guessing but should say exactly what they could see. The participants were asked to read from the top to the bottom (i.e., from the largest prints to the smallest), one eye was tested at a time by occluding the other, and the reverse was done when checking for the second eye. Pupils with visual acuity of >6/12 were considered to have normal vision. Those with the worst visual acuity had pinhole done those with improvement in pinhole-aided visual acuity. The near vision was then checked using the British N chart at 33 cm and those with vision worse than N8 were also considered to have a refractive error. Those pupils with impaired vision had cycloplegic refraction done by the optometrist to determine their refractive status. Children using spectacles also had their visual acuity checked with and without their corrective spectacles. An ocular examination was done by the researcher, the anterior segment of the pupils was examined using a pen torch and loupe X2 was used to examine the everted eyelid for papillae and follicles. Where neccessary to check for cornea abrasion and other pathologies, amethocaine 0.5% was instilled into the eye and a 2 % flourescein dye applied to the lower fornices. The pupils were then asked to blink so that the dye can spread evenly over the cornea surface. The Placido disc was used to check for the presence or absence of keratoconus, whereas ophthalmoscopy was done through an undilated pupil in a semi-dark space. With the child seated a rebound tonometer was used to check the intraocular pressure of each eye and all findings were recorded in the questionnaire.
To avoid interobserver error, using the Cohens kappa, an interobserver reliability test was conducted where a minimum agreement score of 0.8 kappa score was considered reliable.
All pupils whose parents consented and had VKC were included in the study. However, pupils who declined participation and cycloplegic refraction, children with other ocular diseases, and those who had previous ocular surgeries were excluded from the study.
Statistical analysis was done using the Statistical Package for the Social Sciences version 20 (IBM Corporation, Chicago, Illinois, USA). Frequencies and simple percentages were used to analyze the pattern and complications of VKC.
RESULTS
A total of 400 pupils participated in this study. The mean age of the pupils was 8.8 ± 2.9 years and 8.7 ± 3.1 years for males and females, respectively. Males were more in this study with a male-to-female ratio of 1.3:1. VKC was seen in 84 out of the 400 children, resulting in a VKC prevalence of 21.0%. About 2/3rd of the pupils with VKC 51 (60.7%) had a refractive error.
The type of refractive error commonly seen among the pupils with VKC was astigmatism in 31% of the pupils, whereas 39.3% of pupils had a normal state of refraction as shown in [Figure 1].
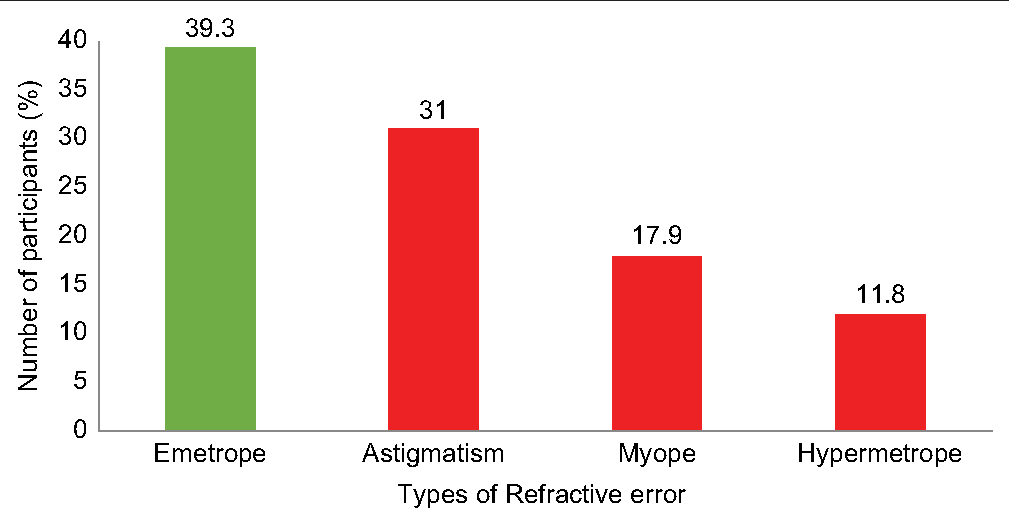
- Distribution of associated refractive error.
The bulbar subtype of VKC is commonly shown in [Figure 2].
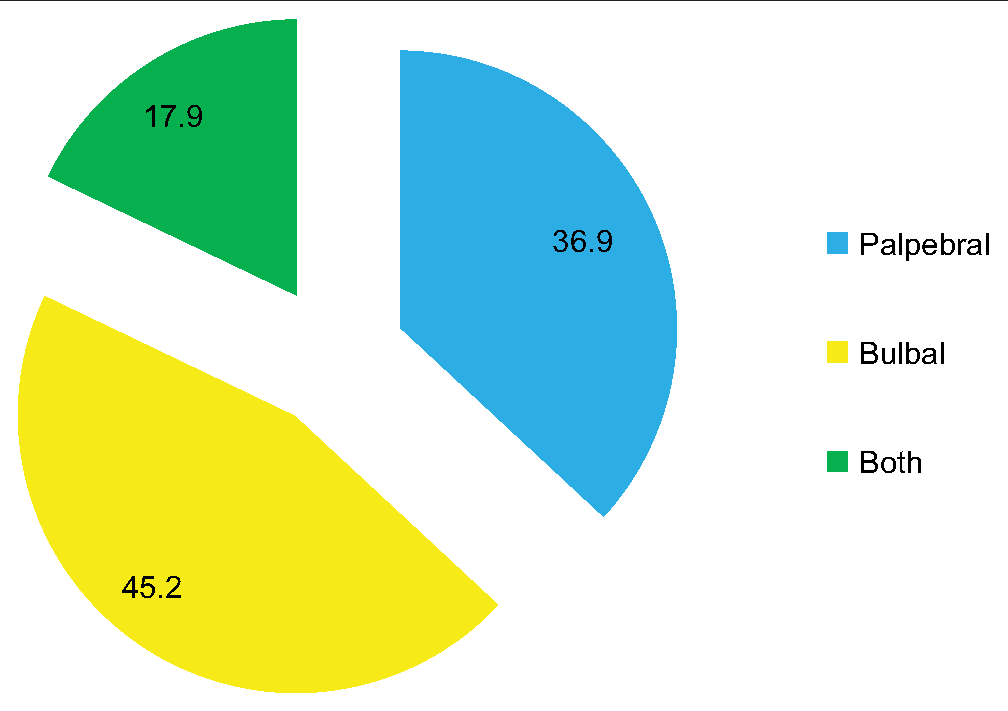
- Type of vernal keratoconjunctivitis.
Refractive error was more common in pupils with the bulbar subtype seen in 38 persons, and astigmatism was common in this group of pupils 19 (50%) as shown in [Table 1].
| Types of Refractive error | Types of VKC | χ2 | p-value | |||
|---|---|---|---|---|---|---|
| Palpebral | Bulbar | Both | Total | |||
| Emetrope | 17 (54.8) | 9 (23.7) | 7 (46.7) | 33 (39.3) | 26.624 | 0.001f |
| Astigmatism | 7 (22.6) | 19 (50.0) | 0 (0.0) | 26 (31.0) | ||
| Myope | 1 (3.2) | 8 (21.1) | 6 (40.0) | 15 (17.9) | ||
| Hypermetrope | 6 (19.4) | 2 (5.3) | 2 (13.3) | 10 (11.9) | ||
| Total | 31 (100.0) | 38 (100.0) | 15 (100.0) | 84 (100.0) | ||
f=Fisher’s Exact Test, VKC: Vernal keratoconjunctivitis
Most of the pupils with VKC and refractive error were in the age group of 5–10 years [Figure 3].

- Correlating vernal keratoconjunctivitis stage with age.
Simple astigmatism was common in the acute VKC stage whereas compound astigmatism was common in the chronic VKC stage as shown in [Table 2].
| Types of Astigmatism | VKC Stages | χ2 | p-value | ||
|---|---|---|---|---|---|
| Acute | Chronic | Total | |||
| Simple | 9 (75.0) | 4 (28.6) | 13 (50.0) | 6.379 | 0.032f |
| Compound | 3 (25.0) | 6 (42.9) | 9 (34.6) | ||
| Mixed | 0 (0.0) | 4 (28.6) | 4 (15.4) | ||
| Total | 12 (100.0) | 14 (100.0) | 26 (100.0) | ||
f=Fisher’s Exact Test, VKC: Vernal keratoconjunctivitis
DISCUSSION
VKC is a chronic, bilateral, and recurrent inflammation of the conjunctiva and cornea.[11] From our study, VKC was seen to be common among the school pupils, and refractive error which is a state that affects the clarity of vision in an individual is a common association in these pupils. This is similar to findings by Wade et al. in the Gambia who also reported that refractive error is one of the most common findings in people with allergic conjunctivitis.[11] Malu in a hospital-based study in Jos also found refractive error to be common in her study among patients with vernal keratoconjunctivitis.[12] Mimura et al. also collaborated on a relationship existing between allergic conjunctivitis and refractive error, they also went further to suggest that refractive error may be a risk factor for allergic conjunctivitis.[13] The association between VKC and refractive error may also be attributed to the change in corneal topography from the chronic inflammation and recurrent itching and rubbing of the eye by individuals who suffer from allergies.[14]
Astigmatism was the most common type of refractive error seen in this study occurring in more than half of those pupils with refractive error, this is similar to findings from other studies.[6,7,15] However, contradicting results were obtained by Shetty et al. in their study, where hypermetropia was found to be the most common refractive error in patients with VKC, just as astigmatism was the least of the refractive errors.[8] Even though we both had similar methodologies, the difference in our findings may be due to differences in the population and geographical area of the studies.
Pupils with the bulbar (limbal) subtype of VKC had a higher frequency of astigmatism; this can be due to the changes that can occur on the cornea because of the area involved in the VKC. Myopia, which is the second most common form of refractive error in our study, was also seen to be common among individuals with the bulbar VKC. This contradicts findings by Shetty et al. who found those with the bulbar (limbal) subtype of VKC to have more hypermetropia as their refractive error and astigmatism being the least.[8] The limbal and mixed forms of VKC are seen more in Africans and Asians, whereas the palpebral form is more common among Americans.[4]
The majority of the pupils seen in our study had the acute form of VKC as compared with the chronic disease. Furthermore, in comparing the stage of the disease with the form of astigmatism seen, more than half of those with simple astigmatism had the acute stage of VKC and this could be because most of the pupils had acute VKC so the curvature changes of the cornea might still be at a milder stage, whereas the compound form of astigmatism was seen more in pupils with the chronic stage of VKC. This is similar to the finding by Shetty et al. who found the compound form of astigmatism to be more common in those with chronic VKC.[8]
CONCLUSION
In our study, we found VKC more in the male population with a male-to-female ratio of 1.3:1 and more common in the 5–10 years age group. Astigmatism was the most commonly associated refractive error followed by myopia. Among the different subtypes of astigmatism, simple astigmatism was seen more often. The acute stage of the disease was seen in most pupils with the bulbar variant of conjunctivitis being more common.
Limitation
This was a cross-sectional study so follow-up of these pupils by further studies will be needed to determine if these refractive errors are a complication of VKC or a simple association of VKC.
Ethical approval
The author(s) declare that they have taken the ethical approval from IRB/IEC.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Vernal keratoconjunctivitis: Atopy and autoimmunity. Eur Rev Med Pharmacol Sci. 2013;17:1419-23.
- [Google Scholar]
- Vernal keratoconjunctivitis: A major review. Acta Ophthalmol. 2009;87:133-47.
- [CrossRef] [PubMed] [Google Scholar]
- Pattern of vernal keratoconjunctivitis and its complications amongst school pupils in Jos East local government areas of Plateau State, North-Central Nigeria. Highland Med Res J. 2022;22:1-6.
- [Google Scholar]
- Vernal keratoconjunctivitis revisited: A case series of 195 patients with long-term follow up. Ophthalmology. 2000;107:1157-63.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic allergic conjunctivitis: An evaluation of the role of family history and atopy. Ann Ibadan Postgrad Med. 2006;4:37-41.
- [CrossRef] [Google Scholar]
- Study of complications and visual impairment in vernal keratoconjunctivitis(VKC) Saudi J Med. 2021;6:1-5.
- [CrossRef] [Google Scholar]
- Pattern of refractive status in patients with vernal keratoconjunctivitis at Birat Medical College Teaching Hospital. JNGMC. 2022;20:n46-8.
- [CrossRef] [Google Scholar]
- A cross-sectional study of refractive error in vernal keratoconjunctivitis. Ophthalmol Appl Sci. 2018;4:59-65.
- [Google Scholar]
- Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ. 2008;86:63-70.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of refractive errors on academic performance of high school Children of Lahore. Front Public Health. 2022;10:869294.
- [CrossRef] [PubMed] [Google Scholar]
- Allergic conjunctivitis at Sheikh Zayed regional eye care center, Gambia. J Ophthalmic Vis Res. 2012;7:24-8.
- [Google Scholar]
- Vernal keratoconjunctivitis in Jos, North-Central Nigeria: A hospital-based study. Sahel Med J. 2014;17:65-70.
- [CrossRef] [Google Scholar]
- Relationship between refraction and allergic conjunctivitis. Eye (Lond). 2009;23:63-6.
- [CrossRef] [PubMed] [Google Scholar]
- Topographic corneal changes in patients with vernal keratoconjunctivitis. Arq Bras Ophtalmol. 2005;68:593-8.
- [CrossRef] [PubMed] [Google Scholar]
- Proportion of refractive errors in patients with vernal keratoconjunctivitis. Ophthalmol Pak. 2013;3:26-9.
- [Google Scholar]






