Translate this page into:
Implementation: Putting guidance into practice

*Corresponding author: Raashi Raj, Indian Health Outcomes, Public Health and Economics Research Centre (IHOPE), Indian Institute of Public Health, Hyderabad, Telangana, India. raashi.raj@iiphh.org
-
Received: ,
Accepted: ,
How to cite this article: Raj R, McGuire H, Pinilla-Dominguez P. Implementation: Putting guidance into practice. IHOPE J Ophthalmol 2022;1:50-2.
Abstract
The implementation of guidance and advice into practice is a crucial step in ensuring that the uptake of guidelines’ recommendations that can contribute to improvements in health outcomes and equitable access to health services. The objective of this paper is to give an understanding of the common barriers to guideline implementation and the evidence-based implementation approach adopted by NICE to overcome these barriers.
Keywords
Evidence based practice
COM-B model
Behavior change wheel
Implementation
INTRODUCTION
The implementation of guidance and advice into practice is a crucial step in ensuring that the uptake of guidelines’ recommendations that can contribute to improvements in health outcomes and equitable access to health services. According to Prof. Richard Grol, “Evidence based medicine should be complemented by the evidence-based implementation.”[1]
The objective of this paper is to give an understanding of the common barriers to guideline implementation and the evidence-based implementation approach adopted by the National Institute for Health and Care Excellence (NICE) to overcome these barriers.
BARRIERS TO IMPLEMENTATION
It is challenging to deliver high-quality and consistent service in health-care systems. Evidence based practice (EBP) promotes the best scientific evidence, patient advocacy, and clinician expertise in health-care delivery. Despite substantial efforts to promote EBP, there has been an ongoing struggle to integrate evidence-based care in health-care systems. Grol and Grimshaw (1997) outlined that the transfer of evidence to clinical practice and decision making is a complex process with a number of decision makers involved. This process requires a meticulous approach at the different levels of care. This approach should be tailored to specific settings and target groups.
Barriers to the successful implementation of guideline recommendations arise from multiple factors categorized at an individual or organizational level. These can be individual barriers, related to the lack of skills of individual staff working in clinical practice and organizational barriers, such as unawareness of implementation techniques or culture, and limited resources.
THE IMPLEMENTATION APPROACH SHOULD BE EVIDENCE BASED
The implementation team at NICE uses evidence-based strategies for implementation and knowledge mobilization (the process of taking knowledge to where it is needed). The strategies used include academic detailing (peer to peer educational outreach), quality improvement, audit and feedback, and service stakeholder engagement. Multi-faceted approaches can have a cumulative and significant effect. Change can only be brought in if people are ready and prepared for it.
Putting evidence into clinical practice is an ongoing process and should not be regarded as a one-off event. Guideline implementation can be unpredictable, and trial-and-error approaches have been shown to be costly and ineffective with variable results. A number of theories, models, and frameworks have been developed to help the implementer maneuver around the many pitfalls to the successful implementation of guidelines.
The COM-B model - Capability, Opportunity, and Motivation and Behavior[2] - is one such model [Figure 1]. This model recognizes that behaviors are part of a system of behaviors with and between people and is encapsulated in the Behavior Change Wheel [Figure 2]. The Behavior Change Wheel encourages the users to choose knowledge translation interventions on a case-by-case basis. The center of the wheel includes sources of behavior: Capability, opportunity, and motivation. Nine intervention functions contribute to these sources of behaviors. In turn, these are surrounded by seven policy categories that should enable the intervention to occur. Interventions can then be designed to bring about a change in practice based on the identification of specific barriers and facilitators.
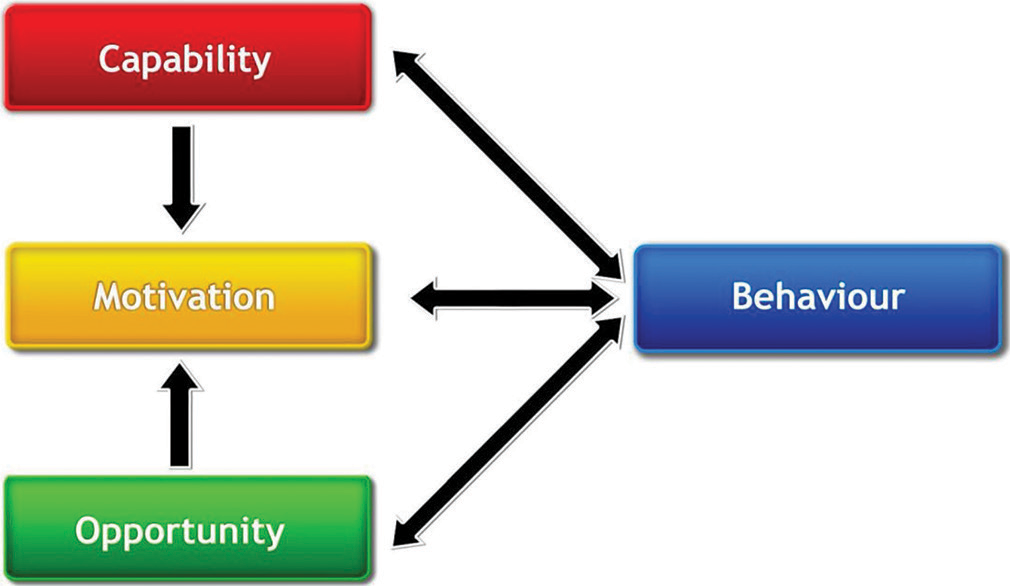
- The COM-B system - a framework for understanding behavior. (Taken from Michie, S., vanStralen, M.M. and West, R. The behavior change wheel: A new method for characterizing and designing behavior change interventions. Implementation Sci 6, 42 (2011). 10.1186/1748-5908-6-42 ).

- The behavior change wheel. (Taken from Michie, S., van Stralen, M.M. and West, R. The behavior change wheel: A new method for characterizing and designing behavior change interventions. Implementation Sci 6, 42 (2011). 10.1186/1748-5908-6-42 ).
NICE’S IMPLEMENTATION APPROACH
The current NICE approach to implementation has been shaped by the NICE Strategy 2021–2026 (https://ihopejournalofophthalmology.com/current-issue/ ) and NICE’s previous experiences. The NICE strategy starts with NICE adopting a “Living” guideline approach as follows:
Develop living guidance
NICE guidance and standards should be focused on the audiences’ needs and evolving evidence base.
Build awareness
NICE works to ensure all relevant audiences are aware of the guidance available and the benefits the guidance can deliver when implemented different methods are employed to do this and may include social media, webinars, and podcasts. There should be direct communication with core audiences using regular electronic and digital platforms.
Motivate
NICE motivates people and organizations to use the NICE guidelines by clearly outlining the benefits of doing so, for example, the guidance will improve the quality of care or lead to efficient use of scarce resources. NICE works with key partners to implement the guidance. For example, NICE works with organizations that regulate professional practice to include the use of NICE guidelines as part of the annual revalidation process.
Practical support
NICE provides practical support for local and national adoption of NICE guidance such as “how to” guides, shared learning examples, audit tools, providing information on resource impact, and social care quick guides.
Evaluate
NICE guidelines uptake should be evaluated regularly to check for its impact, however, NICE does not have a formal role and does not receive any funding to monitor uptake. NICE engages with external organizations to obtain data and intelligence on the use of its guidance.
SUMMARY
Evidence-based medicine is considered the best practice in healthcare. Implementation is a key step in ensuring that evidence-based guidelines are being used in practice. Knowledge of barriers and facilitators to the implementation of guidance at both local and national level will help health-care systems and policy makers to address them and sustain a culture of quality improvement.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Personal paper. Beliefs and evidence in changing clinical practice. BMJ. 1997;315:418-21.
- [CrossRef] [PubMed] [Google Scholar]
- The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42.
- [CrossRef] [PubMed] [Google Scholar]






